Regarding the Medicare QMB Program
Medicare Qualified Member Beneficiary (QMB) Program
Yesterday I logged in with a biller from one of my practices who was confused about something she had not seen before when checking eligibility for Medicare patients. Given the fact that patients had until April 1st to change their current Medicare Advantage/Replacement Plan or to change back to traditional Medicare benefits, I assumed this was a part of the issue. As it turned out, this was not the case and the biller and I both learned about a program that neither of us had been aware of before (the Medicare Qualified Member Beneficiary or QMB Program). This program is not new but is being watched closely to assure that providers are in compliance with the terms of patient financial responsibility (or lack thereof).
In a nutshell, patients (beneficiaries) who are enrolled in the QMB Program (qualifying through income level) have no legal obligation to pay Medicare Part A or Part B deductibles, coinsurance, or copays for any Medicare-covered items and services. These patients may still have a secondary insurance (and it’s not always Medicaid), so you need to find out if the patient is enrolled in the QMB program prior to treating and billing in order to flag the patient as “Do not balance bill; QMB.” The OIG is actively searching for practices that are wrongfully balance billing and patients are encouraged to whistle blow when it happens. You may already be aware of this but for those who are not, please make it a point to meet with your staff and billers to discuss the situation.
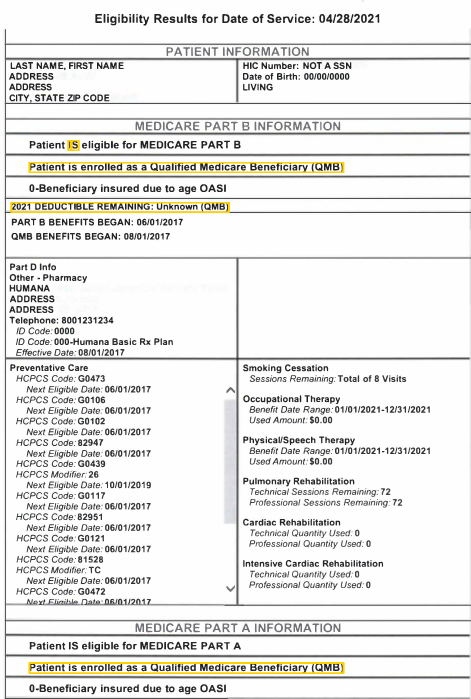
Below you will find a screenshot from the Medicare Provider Portal (with patient information removed) to show what the eligibility screen displays when a patient is enrolled in the QMB Program. Click here for information listed on the CMS website.