E/M Coding Changes for 2021 are Almost Here
What’s your plan?
For more than a year now and especially over the last few months we have been learning about the significant changes to Evaluation and Management (E/M) services set to begin on January 1, 2021. The American Medical Association (AMA), American Podiatric Medical Association (APMA), and an abundance of other medical resource organizations including my own consulting firm Pinnacle Practice Achievement (PPA), have provided countless webinars and articles discussing the ins and outs of these changes and how physicians could prepare for the impact to current workflow.
Here are some examples of questions and concerns expressed to me (maybe they look familiar to you) and my thoughts based on available information and conversations with doctors over the past few months:
• I don’t have a high volume of Medicare patients, should I still change my Medicare coding and documentation practices on January 1st?
Although many podiatry practices are Medicare “heavy” there are instances where Medicare patients account for less than 10%. Many of those physicians have shared a lack of interest in changing their current systems.
• Should I create two new sets of E/M Templates to reflect Medical Decision Making (MDM) or Time Spent?
You can, but keep in mind that you will still need your “old” templates for private payers (who have not committed to these changes), consults and inpatient visits (skilled nursing facilities, hospital visits, etc.). The 2021 E/M changes apply only to outpatient Medicare visits.
Sample chart notes were most recently provided by a panel of APMA experts on December 17th (in a live webinar “Documentation and E/M examples.”). The webinar recording and pdf are available to APMA members by visiting www.APMA.org.
• Is my EHR/Practice Management software ready for these changes?
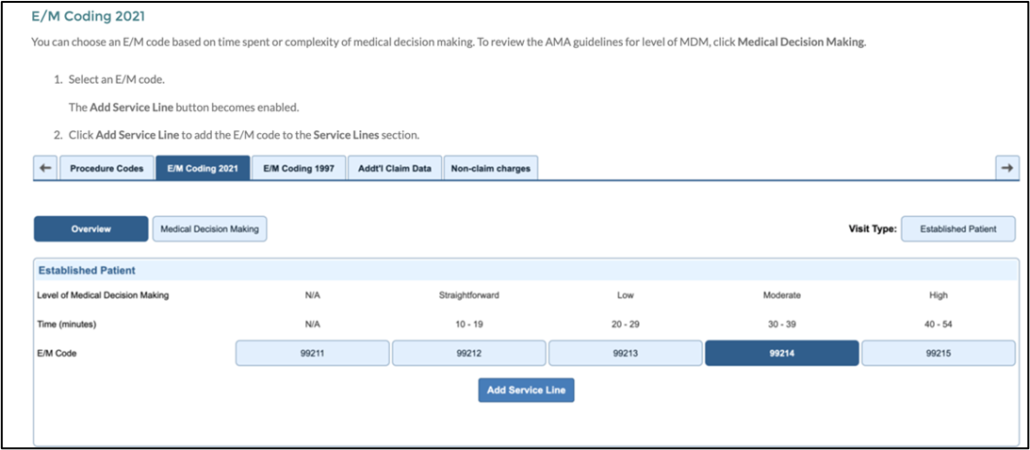
Certified EHRs have been proactive about this change and many are providing tools as pictured here (this is through Nextgen Office; I found it in the Knowledge base tab on the home page by typing “E/M coding and documentation changes 2021”)
• I understand the theory of simplifying documentation in order for physicians to improve their focus on patient care, but what about audits? MDM has always been a point of contention when non-experts review chart notes and compare them to coding. How is this going to be any different?
It is expected that the conversion to MDM as a basis for determining coding level will require major changes to physician behavior and documentation. For each code descriptor for these services in CPT, all references to level of history and physical examination will be removed. In place of the H&P, a medically appropriate history and/or physical examination and a specified level of MDM will be included.
MDM has always been part of the algorithm for choosing a level of service but will now be the sole determinant (unless the provider intends to bill based on time).
As a reminder, MDM in 2021 will be based on:
- Number and complexity of problems addressed
- Amount and/or complexity of data reviewed and analyzed
- Risk of complications and/or mobility or mortality
As a side note, in 2021 when using Time Spent to determine level of service, the length of time corresponding to each level of visit is specified. This may include all related activities “on the day of encounter.” My question as it relates to billing for Time Spent would include consideration for all the doctors who tend to fall behind on documentation): Does this mean that all counseling, correspondence, ordering of tests and charting related to the encounter must be completed on the same day?
I guess we will find out.
• Final question: What should we continue to do as we make our way into the new year and beyond?
Keep up with additional and future proposed changes by using your professional resources (webinars, emails like this, online publications from credible sources, social media forums, etc.).
Share your struggles and findings with colleagues as we work into the new year together.
Determine the want and need to create new templates in your electronic health record system that de-emphasize bullet points for history and exam and emphasize elements of MDM (familiarizing yourself with the definitions of problem types, risks, and other elements of services that will be needed to substantiate it).
Learn to routinely document items within notes that will be used to score MDM, including ordering tests or X-rays, interpreting tests and X-rays, requesting review of outside documents, and having discussions with other healthcare providers.
Use test patients to practice utilizing your new templates/coding levels and self-audit (determine how they would score using the new MDM parameters).
